“The Transitional Heart:” Diagnosis and Treatment of Congenital Heart Disease from the Fetal to Neonatal Stages of Life
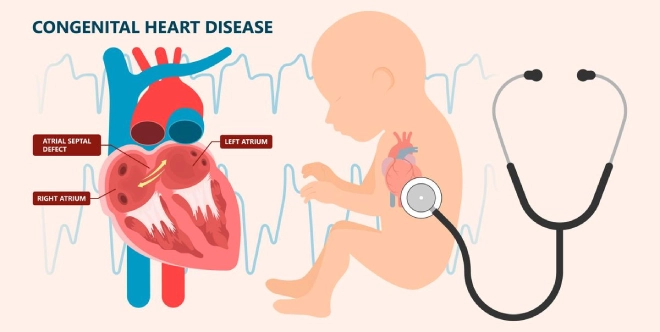
Congenital heart defects (CHD), the most common congenital anomaly, affects nearly one in hundred children in India and is the second-leading cause of infant deaths in low- and middle-income countries. For these reasons, Child Heart Foundation (CHF) is dedicated to improving prenatal diagnosis and management of fetal cardiac abnormalities. While some types of CHD can only be confirmed and treated after birth, many heart problems can be identified during pregnancy, offering a crucial window for early intervention and planning.
The formation of the human heart is an intricate symphony of biological signals, cell migration, and the looping and fusing of heart tubes. With such complex machinery, errors are bound to occur during heart development; these include anatomical and functional issues or problems with the fetal heartbeat. Most common heart defects (e.g., holes between the heart chambers) can be corrected after birth. But certain abnormalities (e.g., narrowing of the valve) are challenging to fix post delivery. In such cases, treatment in utero by maternal administration of drugs or, in rare cases, fetal intervention to prevent abnormal development of pumping chambers can yield maximal chances of survival.
Fetal echocardiography helps repair little hearts
Knowing about a heart problem before birth can enable more effective postnatal care management and help drive optimal long-term health outcomes for children with CHD. Today, with the use of fetal echocardiography many heart malformations can be diagnosed during pregnancy. A routine fetal ultrasound can reveal signs of potential heart defects. This examination may be followed up with a fetal echo around 18-22 weeks of pregnancy to get a more detailed image of the baby’s heart. Following a diagnostic evaluation, healthcare providers and families can assess risk factors and adjust the birth plan accordingly.
A proactive approach to prenatal and postnatal cardiac care
Treatment options for CHD differ based on type and severity as well as occurrence of non-cardiac anomalies. In minor cases where there is no physiological instability medical intervention may be unnecessary. With more complicated cardiac dysfunction, treatment or surgery may be required. For rhythm disturbances, for instance, medication that passes through the placental barrier may be prescribed to the pregnant mother to reduce inflammation and regulate the fetal heartbeat. In cases of an obstructed outlet valve, a balloon catheter may be used to dilate or enlarge the valve. This procedure, using Fetal Image-Guided Surgery, is conducted by placing the catheter into the fetal heart through the mother’s abdominal or uterine wall.
While postnatal instability can be reduced in most newborns with CHD, vulnerable populations with more severe heart conditions can experience high rates of hemodynamic compromise (impaired blood flow) beginning in the delivery room itself. In these situations, risk stratification is essential. A risk-based model can help determine delivery timing and location (e.g., at specialized fetal centers) and appropriate resuscitation and stabilization, including immediate postnatal surgery if required. CHD treatment might include:
- Nonsurgical procedures using a closing device
- Oxygen therapy, which provides higher levels of oxygen than ambient air
- Prostaglandin E1, which relaxes smooth heart muscle and keeps the ductus arteriosus (a blood vessel that normally closes after birth) open, thereby providing circulation
- Surgery to open up or redirect blood flow
- Positioning, drying, and stimulation to facilitate ventilation and perfusion (the passage of fluid)
- Intubation with mechanical ventilation using sedation and neuromuscular blockade
Given advances in fetal surveillance and CHD treatment, the prognosis for neonatal cardiac issues is very positive—90% of children with heart defects survive into adulthood and lead productive, fulfilling lives. At CHF, we are committed to ensuring every family has access to the support, guidance, and resources they need to make informed decisions about their children’s health. Together, we can make sure every child has a healthy heart!
If you or someone you know has concerns about fetal cardiac health and CHD in newborns and infants, don’t hesitate to reach out. Early detection and planning can make all the difference.
Sources
- Arshad, S., et al. (2019). Prenatal detection of congenital heart disease: A review of imaging modalities and diagnostic techniques. PMC National Library of Medicine. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7078965/
- Aster Hospitals. (n.d.). Difference between anomaly scan and fetal echo. Retrieved from https://www.asterhospitals.in/blogs-events-news/aster-women-children-bangalore/difference-between-anomaly-scan-and-fetal-echo
- Calkins, H., & Choi, M. (2023). The transitional heart: From early embryonic and fetal development to postnatal circulation. Fetal Developmental Topics, 47(5), 373–385. Retrieved from https://karger.com/fdt/article/47/5/373/136983/The-Transitional-Heart-From-Early- Embryonic-and
- Cleveland Clinic. (n.d.). Congenital heart disease: Management and treatment. Retrieved from https://my.clevelandclinic.org/health/diseases/21674-congenital-heart-disease#management-and-treatment
- Healthline. (2021). Fetal echocardiography: What it is and why it’s done. Retrieved from https://www.healthline.com/health/fetal-echocardiography
- Johns Hopkins Medicine. (2023, November 16). High-risk neonatal cardiac deliveries clinical pathway. Retrieved from https://www.hopkinsmedicine.org/-/media/files/allchildrens/clinical-pathways/high-risk-neonatal-cardiac-deliveries-clinical-pathway-11_16_23.pdf
- Mayo Clinic. (n.d.). Congenital heart defects in children: Diagnosis and treatment. Retrieved from https://www.mayoclinic.org/diseases-conditions/congenital-heart-defects-children/diagnosis-treatment/drc-20350080
- McLennan, C. (2021). Congenital heart disease in the fetus: Diagnosis and management. Pediatric Development, 33(5), 374–384. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/10.1002/pd.6617
- National Health Service (NHS). (n.d.). Congenital heart disease: Diagnosis. Retrieved from https://www.nhs.uk/conditions/congenital-heart-disease/diagnosis/
- Orvin, J. A., et al. (2020). Cardiovascular evaluation of newborns with congenital heart defects: Prenatal detection and postnatal management. PMC National Library of Medicine. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8429868/
- University of California, San Francisco (UCSF). (n.d.). Congenital heart disease in the fetus: Diagnosis and management. Retrieved from https://fetus.ucsf.edu/congenital-heart-disease/
- UpToDate. (n.d.). Congenital heart disease: Prenatal screening, diagnosis, and management. Retrieved from https://www.uptodate.com/contents/congenital-heart-disease-prenatal-screening-diagnosis-and-management
- Stanford Children's Health. (n.d.). Fetal echocardiography. Retrieved from https://www.stanfordchildrens.org/en/topic/default?id=fetal-echocardiography-90-P01789
Stay Connected
Stay connected for updates, insights, and exciting news delivered directly to you.
Recent Post
-
May 21, 2025
-
Mar 12, 2025



