Why Choose Child Heart Foundation?
Choosing the right support system when your child is diagnosed with a heart condition can be overwhelming. With the growing number of congenital heart disease (CHD) cases in India, especially among children from underprivileged backgrounds, families often find themselves stuck between long waiting periods in public hospitals and unaffordable treatment costs in private ones. In such situations, the question “Why choose CHF?” becomes highly relevant—and the answer is both practical and powerful.
Child Heart Foundation (CHF) is a registered NGO committed solely to the cause of children with heart problems. Its focus is clear: no child should suffer or die due to heart disease just because their family cannot afford treatment. This mission reflects in all its programs, outreach, and partnerships.
One of CHF’s major strengths is its dedication to early diagnosis. Through the PraDAAN® Pediatric Echocardiography Program, the organization offers free or subsidized echo screenings for children up to 18 years of age. These screenings are vital for detecting CHD symptoms early—symptoms that can be subtle and often missed in routine checkups. For families that live far from specialized hospitals or face delays in public healthcare systems, this program can be life-changing.
But diagnosis is just the beginning. Why choose CHF? Because their involvement doesn’t stop there. With the HRIDAAN® Financial Assistance Program, CHF supports children whose families can’t bear the cost of surgery or cardiac procedures. Beyond financial support, CHF helps parents understand their child’s condition, guides them through the hospital admission process, and even follows up post-treatment to ensure proper recovery.
CHF also addresses logistical struggles through SAHYOG, a program that helps with travel, medicines, lodging, and meals—things that many families from outside the city find difficult to manage during prolonged hospital visits.
Their efforts go beyond direct treatment. Why choose CHF? Because they also focus on prevention and awareness. Programs like SUGYAAN® and JEEVANSH® create awareness about heart health in communities and among pregnant women, ensuring that families are better informed and prepared. CHF conducts workshops with frontline health workers, organizes camps in schools and orphanages, and collaborates with government hospitals to make healthcare more accessible.
CHF doesn’t work in isolation. They’ve partnered with some of the most trusted government institutions and have trained doctors in pediatric cardiology through their HRIDYA SAKSHAM initiative. By building local capacities and donating echocardiography machines, CHF is also contributing to long-term improvements in India’s public health infrastructure.
rom awareness to diagnosis, from surgery to recovery, from the hospital bed to home, CHF is not just an organization. It’s a partner in healing.

How CHF Helps Underprivileged Families Manage Pediatric Heart Problems
For underprivileged families in India, accessing timely and quality healthcare can be incredibly challenging—especially when it comes to serious conditions like congenital heart disease (CHD). The cost of diagnosis, treatment, and follow-up care can be financially overwhelming. Add to that the lack of awareness about symptoms or available support, and many children are left undiagnosed or untreated. In this context, understanding how CHF helps underprivileged families becomes important.
Child Heart Foundation (CHF) has designed its programs specifically to address these very issues—working at the ground level to support families from the first signs of a health concern all the way through treatment and recovery. The journey begins with early detection. CHF’s PraDAAN® program provides free or subsidized pediatric echocardiography screenings, helping identify children with heart abnormalities. For many families, this is the first time they’re able to access such a test without long waits in public hospitals.
Once a diagnosis is confirmed, how CHF helps underprivileged families becomes even more evident. Through the HRIDAAN® program, CHF offers financial assistance for heart surgeries and other critical treatments. This is particularly crucial in cases where immediate intervention can save a child’s life and improve their long-term quality of health.
But CHF’s role doesn’t end at funding procedures. The SAHYOG initiative addresses the often-overlooked yet essential aspects of care, such as travel, medication, temporary accommodation, and meals. These logistical challenges can be a major hurdle, especially for families coming from rural areas or smaller towns.
CHF also puts effort into building awareness. Through the SUGYAAN® program, community sessions and partnerships with frontline workers spread information about symptoms of CHD and the availability of services. Additionally, JEEVANSH® offers free fetal echocardiography to pregnant women, allowing early detection and planning before the baby is even born.
These combined efforts create a support system that is both medical and human. CHF’s partnerships with hospitals, NGOs, and local authorities ensure a seamless flow of referrals and follow-ups. So, how CHF helps underprivileged families is not just by offering treatment—it’s by standing beside them through every stage, providing clarity, support, and care.

Top NGO for Heart Problems in Children – Why CHF Stands Out
When it comes to finding the top NGO for heart problems in children, it’s important to look beyond popularity and focus on long-term impact, accessibility, and quality of support. In India, where over 180,000 children are born with congenital heart disease (CHD) every year, timely intervention is essential—but access remains a problem for many underprivileged families.
Child Heart Foundation (CHF) has gradually become recognized as a top NGO for heart problems in children, and not just because of the number of children they’ve helped. What truly makes CHF stand out is the way their entire model is built around early diagnosis, financial support, and community awareness—all tailored to low-income families.
The process starts with their PraDAAN® Pediatric Echocardiography Program, which provides free and discounted heart screenings. In India, many families can’t afford these tests privately, and government hospitals are often overcrowded. CHF’s intervention helps detect CHD early, increasing the chances of successful treatment.
Following diagnosis, CHF steps in with HRIDAAN®, which offers financial assistance for surgeries and cardiac treatments. This eliminates the biggest barrier—cost. So far, they’ve helped hundreds of children receive life-saving interventions. They don’t just fund surgeries—they guide families through hospitals, ensure paperwork is complete, and provide emotional support throughout.
Being a top NGO for heart problems in children also means addressing post-surgery needs. CHF’s SAHYOG program helps with the cost of medicines, travel, and accommodation for outstation families. This is especially helpful for those who have to visit cities like Delhi for treatment from rural areas.
CHF also focuses on early prevention through the JEEVANSH® program, which offers fetal echocardiography during pregnancy, and awareness programs like SUGYAAN®, which have reached over 5,00,000 people. These initiatives build awareness about heart health, so families can act before problems become emergencies.
CHF also contributes to improving the overall healthcare system. Through HRIDYA SAKSHAM, they train pediatricians in echocardiography and donate machines to government hospitals—filling critical gaps in India’s pediatric cardiac infrastructure.
In short, what makes CHF a top NGO for heart problems in children is its consistent, well-rounded approach: from diagnosis to recovery, from education to system-building. CHF doesn’t just offer services—they make sure every child, regardless of their background, has a real shot at a healthy future.

Cardiological Care for Children
The heart is the powerhouse of the body. But what happens when this vital organ fails? How do heart problems specifically affect children and adolescents? The following article provides an overview of causes, symptoms, and treatment for heart disease among our younger populations.
A healthy heart functions like a well-oiled machine. Triggered by electrical signals, the heart chambers expand and relax, the valves open and close like house gates, each muscular section, tissue layer, and cell working in sync to send a surge of blood to the rest of the body. There are times, however, when this intricate machinery stalls. While cardiac illnesses occur more frequently in adults, young children and teenagers experience heart problems too. These disorders can be congenital (present at birth) or acquired.
The importance of early intervention in congenital heart disease cases
Congenital heart disease (CHD) impacts nearly one in hundred children worldwide. These structural malformations are present at birth, and are the most common cause of pediatric heart failure. The two types of CHD are cyanotic (low blood oxygen levels) and acyanotic (abnormal heart pumping).
- Causes: CHD occurs because the fetal heart does not develop properly in the uterus. The exact causes of CHD are unclear but contributing factors may include: inherited abnormal chromosomes or genes; alcohol and drug consumption during pregnancy; and illness during pregnancy.
- Symptoms: While most heart defects can be diagnosed prenatally or post-delivery, some forms of CHD may be detected later in childhood or adolescence. Clinical signs of CHD in younger kids and teens may include: fainting, dizziness, shortness of breath, fatigue, and inability to engage in physical activity.
- Treatment: To effectively treat CHD, early detection is vital. Regular monitoring allows for timely intervention, which helps preclude CHD-related health complications and provides the best chance for children with CHD to live an active, healthy life. Simple CHD conditions can be healed with medication that prevents blood clots or controls irregular heartbeat. More serious CHD cases require medical intervention. Treatment modalities can encompass: cardiac catheterization, corrective surgery, implantable heart device (e.g., a pacemaker or implantable cardioverter defibrillator), and, in rare cases, heart transplantation.
Acquired heart disease: types and treatment
Pediatric acquired heart problems are not present at birth; they arise later in life. As with CHD, acquired heart defects can be caused by viral or bacterial infection, inherited heart conditions, and structural defects, which can put children at higher risk of developing acquired cardiovascular issues. There are four types of acquired heart disease:
- Kawasaki disease: Most common in young children, Kawasaki disease is inflammation of the blood vessels.
- Symptoms: A fever greater than 102.2 degrees Fahrenheit for five or more days alongside at least four of the following: rash, enlarged lymph nodes, swollen red skin on the hands and feet, bloodshot eyes, cracked lips, and a swollen tongue.
- Treatment: Medical therapy within ten days of exhibiting symptoms is necessary to reduce lasting damage to the arteries. Kawasaki disease is usually treated with intravenous gammaglobulin (immunoglobulin). In the ensuing weeks, a child may also be prescribed low-dose aspirin to reduce the risk of blood clotting.
- Myocarditis: Thickening of the heart’s muscular walls, which is often caused by an immune response to viral infection.
- Symptoms: Older children present fewer, more subtle symptoms of myocarditis than newborns and infants. These signs may include: chest pain, heart palpitations, cough, fatigue, fever, belly pain, nausea, and inability to engage in physical activity.
- Treatment: There is no direct cure for myocarditis; instead the focus of treatment is to address the underlying illness as well as support heart functioning and blood circulation. Potential treatment options involve: medication to control blood pressure, intravenous immunoglobulin to reduce inflammation, and complete bed rest.
Rheumatic heart disease: Caused by damage to the heart valves as a result of rheumatic fever, rheumatic heart disease is the most common acquired heart disease in people under the age of 25.
- Symptoms: Clinical presentation of rheumatic heart disease can include chest pain, shortness of breath, swelling of the stomach, hands or feet, fatigue, and rapid or irregular heartbeat.
- Treatment: In severe cases, surgery is required to repair or replace the damaged heart valves; this may be supplemented with blood thinners and medication for heart rhythm abnormalities.
Cardiomyopathy: A chronic heart condition where the heart muscles deteriorate (by thickening or rigidifying) or the heart chambers distend. Apart from genetics and viral infection, cardiomyopathy can also be triggered by metabolic, mitochondrial, or systemic diseases, toxins, and chemotherapy drugs.
- Symptoms: Affected children may complain of shortness of breath, dizziness, rapid heartbeat, bloating, chest pain, and fatigue.
- Treatment: Cardiomyopathy can be managed by administering angiotensin-converting enzyme inhibitors, diuretics and beta blockers to fortify the heart’s pumping capacity; performing a myectomy to remove excess heart muscle; inserting ventricular assist devices; and, in rare cases, conducting a heart transplant.
Managing heart disease in teenagers—it takes a village
Adolescence is a turbulent period even in the best of situations. Add heart defects to the picture, and you can imagine the anxiety and stress a teenager with a heart malady might experience. Given the unique developmental needs of adolescents, a holistic and tailored heart health approach is necessary. As Paul et al notes, teens with CHD are at greater risk of mental health disorders, neurodevelopmental impairments, differences in sexual development, and cardiovascular illness. A multidisciplinary team is required to support teens as they confront myriad challenges in their recovery as well as empower them with the knowledge to build a healthy life. In addressing the pediatric community, Dr. Kriti Puri states: “It take[s] a village to help these patients thrive…This is our call to action, partnering with these young adults and their families, to equip them with the GPS to route them to their optimal outcomes.”
Sources
- American Academy of Pediatrics. (n.d.). Care of the adolescent with congenital heart disease: Beyond the life expectancy. Retrieved from https://publications.aap.org/journal-blogs/blog/24902
/Care-of-the-Adolescent-with-Congenital-Heart
- Better Health Channel. (n.d.). Heart disorders - acquired - children. Better Health Channel. Retrieved from https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/heart-
- Better Health Channel. (n.d.). Kawasaki disease. Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/kawasaki-disease/symptoms-causes/syc-20354598
- Cardiovascular Health, Cleveland Clinic. (n.d.). Heart failure in children and adolescents. American Heart Association. Retrieved from https://www.heart.org/en/health-topics/heart-failure
/what-is-heart-failure/heart-failure-in-children-and-adolescents
- Cincinnati Children's Hospital Medical Center. (n.d.). Myocarditis. Retrieved from https://www.cincinnatichildrens.org/health/m/myocarditis
- Cleveland Clinic. (n.d.). Congenital heart disease. Retrieved from https://my.clevelandclinic.org/
health/diseases/21674-congenital-heart-disease#overview
- Cleveland Clinic. (n.d.). Pediatric cardiology. Retrieved from https://my.clevelandclinic.org/
- HealthyChildren.org. (n.d.). Pediatric cardiomyopathy. American Academy of Pediatrics. Retrieved from https://www.healthychildren.org/English/health-issues/conditions/heart/
- Mayo Clinic. (n.d.). Congenital heart defects in children. Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/congenital-heart-defects-children/symptoms-causes/syc-20350074
- Medanta. (n.d.). The importance of pediatric cardiology in early childhood. Medanta - The Medicity. Retrieved from https://www.medanta.org/patient-education-blog/the-importance-of-
- Modern Heart and Vascular. (n.d.). Heart disease in children and teens. Retrieved from https://www.modernheartandvascular.com/heart-disease-in-children-and-teens/
- Mount Sinai Health System. (n.d.). Care of the adolescent with congenital heart disease: Beyond the life expectancy. Retrieved from https://scholars.mssm.edu/en/publications/care-of-the-
adolescent-with-congenital-heart-disease-beyond-the-l
- National Heart, Lung, and Blood Institute. (n.d.). Care of the adolescent with congenital heart disease: Beyond the life expectancy. Retrieved from https://scholars.mssm.edu/en/publications/
care-of-the-adolescent-with-congenital-heart-disease-beyond-the-l
- Oregon Health & Science University. (n.d.). Congenital heart defects in children. OHSU. Retrieved from https://www.ohsu.edu/doernbecher/congenital-heart-defects-children
- PubMed Central. (2021). Pediatric cardiology and heart disease: An overview. National Institutes of Health. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8996670/
- Public Health Agency of Canada. (n.d.). Rheumatic heart disease. World Health Organization. Retrieved from https://www.who.int/news-room/fact-sheets/detail/rheumatic-heart-disease#:~:text
=It%20most%20commonly%20occurs%20in,antibiotics%20when%20they%20do%20occur
- Temple Health. (n.d.). 10 interesting heart facts you may not know. Temple Health. Retrieved from https://www.templehealth.org/about/blog/10-interesting-heart-facts-you-may-not-know
- University of California, Davis Health. (n.d.). Acquired heart conditions in children. UC Davis Health. Retrieved from https://health.ucdavis.edu/conditions/pediatrics/pediatric-cardiology/

Congenital Heart Defects in Newborns and Infants: India’s ‘Invisible’ Illness
Child Heart Foundation sheds light on congenital heart defects (CHD) and how they affect children at the beginning of life.
When we think about heart ailments, perhaps what comes to mind is the image of an old, infirm body or morbid obesity. What we do not picture is a newborn baby—those chubby-cheeked cherubs who are pure delight. In reality, however, one in every hundred infants is born with congenital heart disease (CHD). In India, CHD is the third leading cause of infant mortality. Nearly 240,000 babies are born with CHD annually, of which 60,000 cases are critical and require surgery. Yet, as Dr. Ganesh Mani describes, CHD is the “forgotten” heart disease in India: only one in four children who require heart surgery get the care they need. The problem lies more in access than treatment. In the United States, for example, the Center for Disease Control and Prevention reports survival rates of 95% and 69% in neonatal populations with noncritical CHD and critical CHD respectively. In contrast, in India, 90% of children with serious CHD do not get quality healthcare. A study conducted by Banothu et al found a mortality rate of 50% among 58 children with unoperated CHD in pediatric intensive care units. A number of factors underlie this health crisis: financial constraints, lack of infrastructure and expertise, and inadequate sensitization to the importance of early diagnosis and intervention.
Little baby Rudra was diagnosed with ventricular septal defect and pulmonary atresia, a life-threatening disease. Regular follow-up visits and screenings are vital to monitor Rudra’s condition until he is ready for surgery.
What is CHD and what causes it?
CHD are structural problems that arise due to abnormal malformations of the heart or major blood vessels during the first eight weeks of fetal development. CHD ranges from simple (e.g., holes between the heart chambers) to complex (e.g., the absence of a heart chamber). Doctors do not know what exactly causes CHD but risk factors may include: genetics, alcohol consumption and smoking, and drug use during pregnancy. While there are numerous types of CHD, the most common are:
- Aortic valve stenosis: a valve that does not close and leaks blood
- Coarctation of the aorta: a narrowing of the aorta
- Ebstein's anomaly: a malformed heart that does not pump blood in the right direction
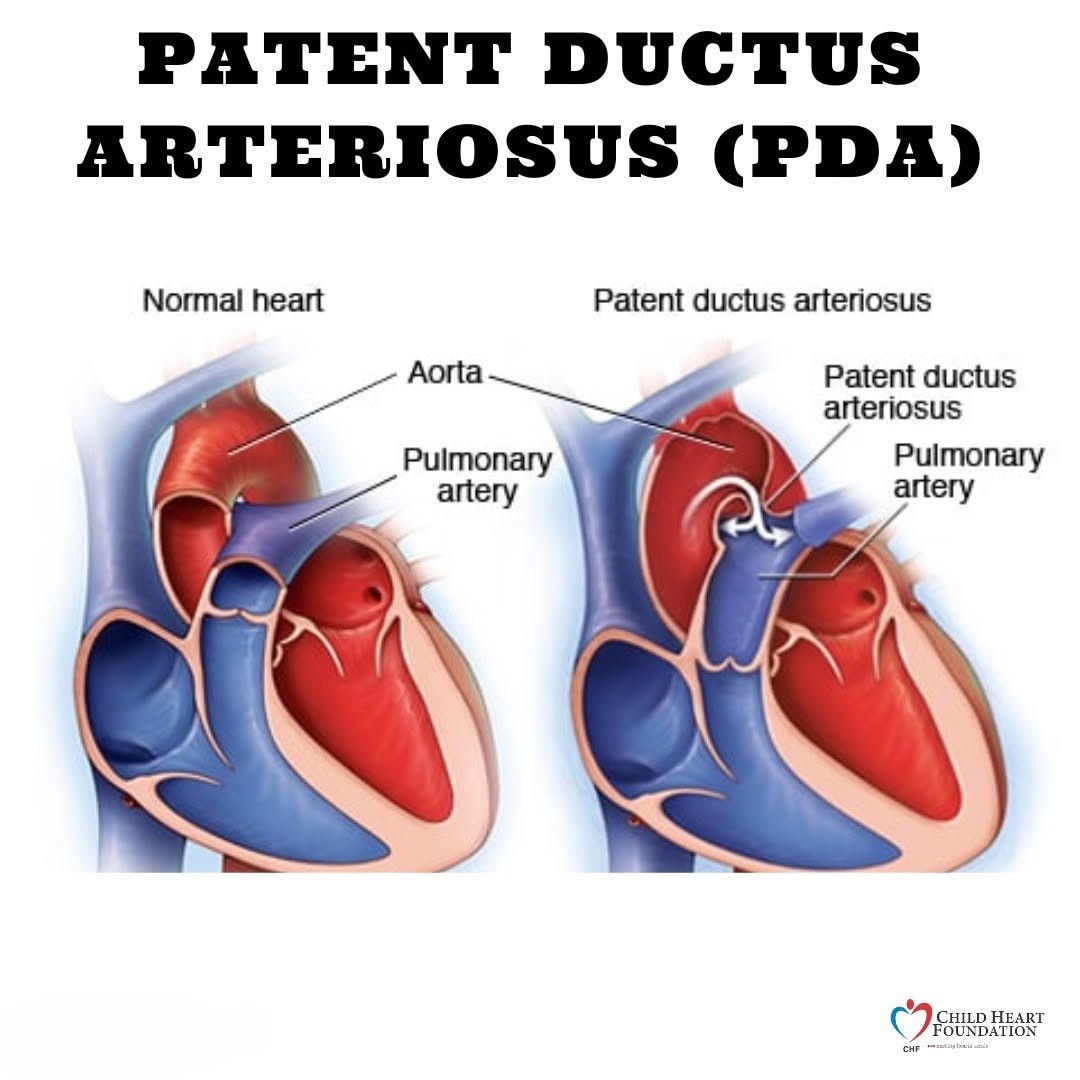
- Patent ductus arteriosis: a hole in the aorta
- Pulmonary valve stenosis: a thickened or fused heart valve
- Septal defects: holes between the heart walls
Diagnosing CHD in newborns and infants
Some cases of CHD do not cause any symptoms and may not even be diagnosed until adolescence or adulthood; others are detected before birth or immediately post-delivery. Key symptoms can encompass:
- Bluish skin, lips or nails
- Excessive sleepiness
- Fast breathing or trouble breathing
- Fatigue
- Heart murmurs
- Weak pulse or pounding heartbeat
Birth can be jarring for babies. They are thrust from the dark, warm amniotic sac into the bright lights of the world. No longer cocooned, the baby cannot depend on the mother for nutrients and oxygen. A baby’s first breath triggers a cascade of changes, including in how the heart pumps blood to the rest of the body. Heart defects can hamper this transition.
Clinical presentation of CHD in newborns can be challenging to pinpoint. Early screening, therefore, is key. In the first few days after birth, neonatal infants should be checked for CHD using a pulse oximeter, which measures blood oxygen levels. Low blood oxygen levels may be a sign of CHD. Further evaluations may be conducted to confirm a diagnosis, including:
- Physical examination: a stethoscope is used to check for a heart murmur or abnormal heartbeats
- Chest X-ray: provides a visual of structural abnormalities
- Electrocardiogram: detects the heart’s electrical activity
- Echocardiogram: creates images of the heart’s valves and chambers
- Cardiac catheterization: a test where a thin, hollow tube is guided through a blood vessel to the heart. This procedure can be used to identify anatomic deviations that are difficult to capture in an echo. Catheterization is also a treatment modality to fix simple cardiac defects.
- Magnetic resonance imaging: generates detailed structural pictures of the heart, enabling accurate measurements of the heart chambers
The importance of early intervention in treating CHD
Most CHD problems are mild and can be managed through regular monitoring in an outpatient setting. However, infants with critical CHD need medical therapy within the first year of life. Untreated cases can lead to a host of complications: heart failure, blood clots, abnormal heart rhythms, stroke, liver disease, kidney failure, pulmonary hypertension, and heart valve disease. Severe defects require medication (e.g., digoxin to slow the heartbeat and boost heart pumping, diuretics to flush out fluid from the body, etc.) or corrective surgery. For complex defects that cannot be repaired surgically, a heart transplant may be necessary. But newborns and infants who are too small or weak are not good candidates for heart surgery. In these situations, palliative surgery may be employed as a stopgap to increase oxygen levels until the baby is ready for cardiac surgery.
A CHD diagnosis can be anxiety-inducing. But medical advances have made early detection and management possible, giving the best chance for your little one to live a long, healthy life. At the Child
Heart Foundation, we are committed to making this vision a reality in India. By raising awareness about best practices, training frontline healthcare workers in timely detection, and advocating for every child to get the support they need, we strive to close gaps in access to quality pediatric heart care. After all, every heartbeat matters.
Sources
- American Heart Association. (n.d.). About congenital heart defects. Retrieved from https://www.heart.org/en/health-topics/congenital-heart-defects/about-congenital-heart-defects
- American Heart Association. (n.d.). Common types of heart defects. Retrieved from https://www.heart.org/en/health-topics/congenital-heart-defects/about-congenital-heart-defects/common-types-of-heart-defects#:~:text=Jackson%20was%20born%20with%20tricuspid,once%20thought%20to%20be%20hopeless
- Children's HeartLink. (n.d.). Where we work: India. Retrieved from https://childrensheartlink.org/global-impact/where-we-work/india/
- Children's HeartLink. (2025). India fact sheet. Retrieved from https://childrensheartlink.org/wp-content/uploads/2025/02/India-Fact-Sheet.pdf
- Cleveland Clinic. (n.d.). Congenital heart disease. Retrieved from https://my.clevelandclinic.org/health/diseases/21674-congenital-heart-disease
- Eternal Hospital. (n.d.). Congenital heart disease and its types. Retrieved from https://www.eternalhospital.com/title/congenital-heart-disease-and-its-types#:~:text=Considering%20a%20birth%20prevalence%20of,the%20first%20year%20of%20life
- Grover, S. (2022). Mortality in congenital heart diseases: Review and progress in improving outcomes. Journal of Clinical Medicine, 41(3). Retrieved from https://doi.org/10.1007/s12098-022-04343-5
- Hindustan Times. (2021). India’s children and the grim reality of congenital heart diseases. Retrieved from https://www.hindustantimes.com/opinion/indias-children-and-the-grim-reality-of-congenital-heart-diseases-101633330205860.html
- Indian Pediatrics. (2018). Congenital heart defects in children: A review of current trends in diagnosis and management. Indian Pediatrics, 55(12), 1075-1082. Retrieved from https://www.indianpediatrics.net/dec2018/dec-1075-1082.htm
- IJPediatrics. (2021). Congenital heart defects: A growing concern in children. Indian Journal of Pediatrics, 88(4), 135-145. Retrieved from https://www.ijpediatrics.com/index.php/ijcp/article/view/4268
- Johns Hopkins Medicine. (n.d.). Care of the baby in the delivery room. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/care-of-the-baby-in-the-delivery-room#:~:text=The%20birth%20of%20a%20baby,from%20the%20nose%20and%20mouth
- Max Healthcare. (n.d.). Congenital heart defects in children. Retrieved from https://www.maxhealthcare.in/blogs/congenital-heart-defects-in-children
- Mayo Clinic. (n.d.). Cardiac catheterization. Retrieved from https://www.mayoclinic.org/tests-procedures/cardiac-catheterization/about/pac-20384695
- Mayo Clinic. (n.d.). Congenital heart defects in children: Diagnosis and treatment. Retrieved from https://www.mayoclinic.org/diseases-conditions/congenital-heart-defects-children/diagnosis-treatment/drc-20350080
- Morrow, W. R., & Sargent, R. (2011). Congenital heart disease in the newborn requiring early intervention. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3145901/#sec25
- National Heart, Lung, and Blood Institute. (n.d.). Congenital heart defects. Retrieved from https://www.nhlbi.nih.gov/health/congenital-heart-defects
- National Heart, Lung, and Blood Institute. (n.d.). Treatment for congenital heart defects. Retrieved from https://www.nhlbi.nih.gov/health/congenital-heart-defects/treatment
- NHS. (n.d.). Types of congenital heart disease. Retrieved from https://www.nhs.uk/conditions/congenital-heart-disease/types/
- The Conversation. (2022). Curious kids: Why do babies cry when they come out of their mum? Retrieved from https://theconversation.com/curious-kids-why-do-babies-cry-when-they-come-out-of-their-mum-205477
“The Transitional Heart:” Diagnosis and Treatment of Congenital Heart Disease from the Fetal to Neonatal Stages of Life
Congenital heart defects (CHD), the most common congenital anomaly, affects nearly one in hundred children in India and is the second-leading cause of infant deaths in low- and middle-income countries. For these reasons, Child Heart Foundation (CHF) is dedicated to improving prenatal diagnosis and management of fetal cardiac abnormalities. While some types of CHD can only be confirmed and treated after birth, many heart problems can be identified during pregnancy, offering a crucial window for early intervention and planning.
The formation of the human heart is an intricate symphony of biological signals, cell migration, and the looping and fusing of heart tubes. With such complex machinery, errors are bound to occur during heart development; these include anatomical and functional issues or problems with the fetal heartbeat. Most common heart defects (e.g., holes between the heart chambers) can be corrected after birth. But certain abnormalities (e.g., narrowing of the valve) are challenging to fix post delivery. In such cases, treatment in utero by maternal administration of drugs or, in rare cases, fetal intervention to prevent abnormal development of pumping chambers can yield maximal chances of survival.
Fetal echocardiography helps repair little hearts
Knowing about a heart problem before birth can enable more effective postnatal care management and help drive optimal long-term health outcomes for children with CHD. Today, with the use of fetal echocardiography many heart malformations can be diagnosed during pregnancy. A routine fetal ultrasound can reveal signs of potential heart defects. This examination may be followed up with a fetal echo around 18-22 weeks of pregnancy to get a more detailed image of the baby’s heart. Following a diagnostic evaluation, healthcare providers and families can assess risk factors and adjust the birth plan accordingly.
A proactive approach to prenatal and postnatal cardiac care
Treatment options for CHD differ based on type and severity as well as occurrence of non-cardiac anomalies. In minor cases where there is no physiological instability medical intervention may be unnecessary. With more complicated cardiac dysfunction, treatment or surgery may be required. For rhythm disturbances, for instance, medication that passes through the placental barrier may be prescribed to the pregnant mother to reduce inflammation and regulate the fetal heartbeat. In cases of an obstructed outlet valve, a balloon catheter may be used to dilate or enlarge the valve. This procedure, using Fetal Image-Guided Surgery, is conducted by placing the catheter into the fetal heart through the mother’s abdominal or uterine wall.
While postnatal instability can be reduced in most newborns with CHD, vulnerable populations with more severe heart conditions can experience high rates of hemodynamic compromise (impaired blood flow) beginning in the delivery room itself. In these situations, risk stratification is essential. A risk-based model can help determine delivery timing and location (e.g., at specialized fetal centers) and appropriate resuscitation and stabilization, including immediate postnatal surgery if required. CHD treatment might include:
- Nonsurgical procedures using a closing device
- Oxygen therapy, which provides higher levels of oxygen than ambient air
- Prostaglandin E1, which relaxes smooth heart muscle and keeps the ductus arteriosus (a blood vessel that normally closes after birth) open, thereby providing circulation
- Surgery to open up or redirect blood flow
- Positioning, drying, and stimulation to facilitate ventilation and perfusion (the passage of fluid)
- Intubation with mechanical ventilation using sedation and neuromuscular blockade
Given advances in fetal surveillance and CHD treatment, the prognosis for neonatal cardiac issues is very positive—90% of children with heart defects survive into adulthood and lead productive, fulfilling lives. At CHF, we are committed to ensuring every family has access to the support, guidance, and resources they need to make informed decisions about their children’s health. Together, we can make sure every child has a healthy heart!
If you or someone you know has concerns about fetal cardiac health and CHD in newborns and infants, don’t hesitate to reach out. Early detection and planning can make all the difference.
Sources
- Arshad, S., et al. (2019). Prenatal detection of congenital heart disease: A review of imaging modalities and diagnostic techniques. PMC National Library of Medicine. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7078965/
- Aster Hospitals. (n.d.). Difference between anomaly scan and fetal echo. Retrieved from https://www.asterhospitals.in/blogs-events-news/aster-women-children-bangalore/difference-between-anomaly-scan-and-fetal-echo
- Calkins, H., & Choi, M. (2023). The transitional heart: From early embryonic and fetal development to postnatal circulation. Fetal Developmental Topics, 47(5), 373–385. Retrieved from https://karger.com/fdt/article/47/5/373/136983/The-Transitional-Heart-From-Early- Embryonic-and
- Cleveland Clinic. (n.d.). Congenital heart disease: Management and treatment. Retrieved from https://my.clevelandclinic.org/health/diseases/21674-congenital-heart-disease#management-and-treatment
- Healthline. (2021). Fetal echocardiography: What it is and why it’s done. Retrieved from https://www.healthline.com/health/fetal-echocardiography
- Johns Hopkins Medicine. (2023, November 16). High-risk neonatal cardiac deliveries clinical pathway. Retrieved from https://www.hopkinsmedicine.org/-/media/files/allchildrens/clinical-pathways/high-risk-neonatal-cardiac-deliveries-clinical-pathway-11_16_23.pdf
- Mayo Clinic. (n.d.). Congenital heart defects in children: Diagnosis and treatment. Retrieved from https://www.mayoclinic.org/diseases-conditions/congenital-heart-defects-children/diagnosis-treatment/drc-20350080
- McLennan, C. (2021). Congenital heart disease in the fetus: Diagnosis and management. Pediatric Development, 33(5), 374–384. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/10.1002/pd.6617
- National Health Service (NHS). (n.d.). Congenital heart disease: Diagnosis. Retrieved from https://www.nhs.uk/conditions/congenital-heart-disease/diagnosis/
- Orvin, J. A., et al. (2020). Cardiovascular evaluation of newborns with congenital heart defects: Prenatal detection and postnatal management. PMC National Library of Medicine. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8429868/
- University of California, San Francisco (UCSF). (n.d.). Congenital heart disease in the fetus: Diagnosis and management. Retrieved from https://fetus.ucsf.edu/congenital-heart-disease/
- UpToDate. (n.d.). Congenital heart disease: Prenatal screening, diagnosis, and management. Retrieved from https://www.uptodate.com/contents/congenital-heart-disease-prenatal-screening-diagnosis-and-management
- Stanford Children's Health. (n.d.). Fetal echocardiography. Retrieved from https://www.stanfordchildrens.org/en/topic/default?id=fetal-echocardiography-90-P01789

Understanding Heart Murmurs in Children: What Every Parent Needs to Know
Child Heart Foundation provides an overview of diagnosis and treatment of heart murmurs in pediatric cases
Lubb-dupp, lubb-dupp, lubb-dupp—this is the sound of a typical heartbeat. Heart murmurs, in contrast, sound like the whooshing of wind, like water rushing through a pipe. Caused by turbulent blood flow in the heart, murmurs are the extra noise heard between heartbeats. They can be caused when:
- The heart expands and fills with blood: diastolic murmur
- The heart contracts: systolic murmur
- Throughout the heartbeat: continuous murmur
Heart murmurs can present at birth (congenital) or form later in life. They are common in healthy infants, children, and adolescents. Most are benign; some can be pathologic. In the latter case, heart murmurs arise due to congenital heart defects (CHD) or acquired structural heart disease. Symptoms of pathologic heart murmurs can include:
- Poor feeding, eating, or weight gain
- Shortness of breath or breathing fast
- Sweating
- Chest pain
- Dizziness or fainting (syncope)
- Bluish skin, particularly of the lips and fingertips
- Cough
- Swelling (edema) of the lower legs, ankles, feet, abdomen, liver, or neck veins
How are heart murmurs diagnosed in a child?
A healthcare provider will first take a history of your child’s symptoms and health; this will be followed by a physical examination. During the exam, if the clinician hears abnormal heart sounds, they will refer you to a pediatric cardiologist. The cardiologist might order the following tests:
- Chest X-ray: an image of the heart and lungs
- Electrocardiogram (ECG): a record of the heart’s electrical activity
- Echocardiography (echo): an ultrasound to look at the structure and function of the heart. This is the recommended diagnostic method for pathological murmurs.
In most cases, benign murmurs do not indicate structural heart abnormalities, and thus do not require an echo test. However, the threshold for further investigation and referral to pediatric cardiologists is lower for neonates and young infants, given the high rates of CHD in these populations and the association between CHD and asymptomatic murmurs in young children.
Treatment of heart murmurs
While a heart murmur diagnosis in your child may cause anxiety, most heart murmurs are benign and get resolved on their own. Treatment of pathologic heart murmurs will differ based on your child’s symptoms, age, and overall health. If the murmur is caused by CHD, medication (e.g., blood thinners, beta blockers, water pills, and ACE inhibitors) or surgery (e.g., heart valve surgery) might be required to correct the structural heart defect. If the murmur is due to another condition, direct treatment of this underlying issue will usually lead to the heart murmur subsiding.
With regular monitoring and early intervention, most children with heart murmurs go on to lead normal, healthy lives. It is with this goal in mind that Child Heart Foundation works to expand the pediatric cardiac infrastructure in India and increase access to specialized health services for every family. With the right care, your child’s heart can continue to beat strong.
Sources
- Di Nardo, M., & Ho, P. (2012). Pediatric heart murmurs: A practical guide to diagnosis. PubMed Central (PMC). Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3446116/
- Hopkins Medicine. (n.d.). Heart murmurs in children. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/heart-murmurs
- KidsHealth. (n.d.). Heart murmurs in children. Retrieved from https://kidshealth.org/en/parents/murmurs.html
- Loder, E., & Kazzi, A. (2011). Heart murmurs in children. American Family Physician, 84(7), 793–801. Retrieved from https://www.aafp.org/pubs/afp/issues/2011/1001/p793.html
- Mayo Clinic. (n.d.). Heart murmurs: Symptoms and causes. Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/heart-murmurs/symptoms-causes/syc-20373171
- Sidiropoulos, C., et al. (2011). Pediatric heart murmurs: A systematic review. PubMed. Retrieved from https://pubmed.ncbi.nlm.nih.gov/22010618/
- Yip, G., et al. (2024). Cardiac murmurs in children. The Australian Journal of General Practice. Retrieved from https://www1.racgp.org.au/ajgp/2024/july/cardiac-murmurs-in-children
Heart connections : Modern Breakthroughs in treating Patent Ductus Arteriosus (PDA)
Patent ductus arteriosus (PDA) is a heart condition where a small blood vessel, the ductus
arteriosus, fails to close after birth, leading to abnormal blood flow between the main heart
artery (aorta) and primary lung artery (pulmonary artery). This condition is more common in
premature infants but can also affect full-term babies. If left untreated, Patent ductus
arteriosus can lead to problems like:
● Heart failure
● Endocarditis (inflammation and infection of the lining of the heart)
● Pulmonary Edema(fluid in the lungs)
● Pulmonary Hypertension( high blood pressure in the blood vessels of the lungs)
Fortunately, there are several treatment options to address PDA, ranging from medication to
surgical intervention.
The Child Heart Foundation is a non-governmental organisation that provides assistance to
infants who are born with congenital heart problems like patent ductus arteriosus (PDA),
ventricular septal defects (VSD) and other ethical medical conundrums. These conditions
call for early detection, targeted therapies and prolonged treatment all of which is demanding
financially and emotionally for families affected. The aim of CHF is to ease such stresses by
providing a great number of activities which enhance the life and health of the children
suffering from this complexity, particularly the disadvantaged.
The treatment includes:
1. Observation and Monitoring:
In some cases, especially in small PDAs, doctors recommend close observation. Some
PDAs resolve on their own, particularly in younger gestational age patients.
Regular monitoring through echocardiograms and physical examinations are performed to
ascertain the need for other measures.
2. Medication:
Medications like ibuprofen or indomethacin can encourage PDA closure in preterm infants by
reducing the levels of prostaglandins, which keep the ductus arteriosus open. These drugs
are usually effective in infants born prematurely, although they may be less effective in older
or full-term infants.
3. Cardiac Catheterization :
If the PDA does not close on its own or with medication, catheter-based closure is the most
common, minimally invasive approach for the treatment of PDA.
A paediatric interventional cardiologist makes a tiny incision near a large blood vessel in the
leg . A small device, typically a coil or an occluder, is inserted through a catheter (a thin tube)
into the ductus to seal it. This procedure is effective and has a quick recovery time, often
suitable for children and adults with larger PDAs.
4. Patent Ductus Arteriosus Surgery:In cases where other treatments are unsuitable or unsuccessful, surgery may be necessary.
This procedure, called PDA is done by a paediatric heart surgeon who makes an incision in
the chest and then closes the PDA by stitching or clipping it. Although more invasive, it is
highly effective and typically has good outcomes.
Early diagnosis and appropriate treatment of PDA are essential for preventing complications.
Treatment options depend on the patient's age, PDA size, and overall health. Consulting
with a paediatric cardiologist is crucial to determine the best approach for each individual
case. With advanced treatments available, PDA can be effectively managed, allowing most
patients to lead healthy lives.
Most children who have undergone surgical procedures need prolonged follow-up care and
specialised management in order to assess their cardiac health and growth. The Child Heart
Foundation helps families with post-operative care resources, including nutrition and
exercise management, regular medical check-ups, to help ensure that these children
continue to grow as they age.

Common heart conditions in children
Heart conditions in children are medical disorders that affect the structure or function of the heart. These conditions can range from congenital heart defects (CHDs), present at birth, to acquired heart diseases that develop after birth due to infections, inflammation, or other causes. While some heart conditions are mild and resolve without significant intervention, others may require lifelong management, specialized treatments, or surgical correction.
Types of Heart Conditions
1. Congenital Heart Defects (CHDs)
Types of CHDs
Symptoms
2. Acquired Heart Conditions
Rheumatic Heart Disease
Kawasaki Disease
3. Arrhythmias (Irregular Heartbeats)
Types of Arrhythmias:
4. Cardiomyopathies

Urgent Help Needed: Baby Prashant's Fight for Life
Meet Prashant, a 6-month-old baby from a small village in Himachal Pradesh. Prashant’s story is one of love, hope, and a family’s unwavering fight against adversity. He lives with his parents and two elder siblings in a modest household. His father, a street vendor, is the only earning member of the family, bringing home around ₹10,000 per month to support the family.
At just 4 months old, Prashant began showing signs of cold and cough. Concerned, his parents took him to the hospital, where they were devastated to learn that their baby boy was suffering from a congenital heart disease. The diagnosis was a harsh reality for a family already living in challenging conditions. With Prashant's heart condition worsening, the doctors have advised urgent heart surgery to save his life.
However, there's a significant hurdle standing between Prashant and the surgery he so desperately needs — blood. The surgery cannot proceed without a safe supply of blood, and Prashant’s family is struggling to find the resources required for this crucial part of the procedure.
The financial situation of the family makes this even more difficult. Prashant's father is working tirelessly as a street vendor, but the low monthly income leaves little room for medical expenses. The family is reaching out for support, knowing that every drop of blood and every ounce of kindness could make the difference between life and death for their baby boy.
How You Can Help
Blood Donation: Prashant urgently requires blood to undergo surgery. Your donation could save his life. If you're in the area and able to donate, please consider doing so. Your contribution could give Prashant the chance to live a healthy life.
Financial Support: The family also needs assistance with medical expenses. Any financial help, no matter how small, can make a huge impact on Prashant’s treatment and care.
Contact Information for Donation:
📅 Blood Donation Needed: ASAP
📍 Location: Child Heart Foundation
📞 Contact Person for Blood Donation: 9667 608 855, 9773 744 848
Please help us spread the word and provide support to Prashant and his family during this incredibly difficult time. Together, we can make a difference and give this little one the chance to grow up healthy and strong.
Thank you for your compassion and generosity.

Understanding Pulmonary Hypertension: Bridging the gap by providing support & Solution to Children
With the development in medical science, people are aware of the problems associated with various heart diseases, especially children. The condition known as Pulmonary Hypertension (PH) is often overlooked but can have serious consequences. Pulmonary Hypertension is a serious condition characterized by high blood pressure in the pulmonary arteries, which carry blood from the heart to the lungs. This elevated pressure can lead to various complications, including heart failure. In children, PH can be caused by congenital heart defects, lung diseases, or may arise without any identifiable cause (idiopathic). Symptoms of Pulmonary Hypertension are crucial for timely intervention:- Shortness of breath: This may occur during physical activity or even at rest in advanced cases. Fatigue: Children may tire more easily than their peers. Chest pain: Discomfort or pain in the chest can be a concerning sign. Rapid heartbeat: A noticeable increase in heart rate can occur as the heart works harder to pump blood. Swelling: This can manifest in the legs, ankles, or abdomen due to fluid retention. Children from economically disadvantaged families can receive free treatment from CHF. Our belief is that every child deserves a quality life, and we make an effort to prevent financial limitations from obstructing their access to care. The objective of our organisation is to ensure that families can pay for medical expenses, which will enable them to focus on their child's recovery. In addition to other medical institutions, the Child Heart Foundation partners with a network of hospitals and healthcare facilities throughout India that offer paediatric cardiology services. Several of our hospital referrals from Safdarjung Hospital, Lok Nayak Hospital, Sanjay Gandhi Memorial Hospital etc, are highly respected institutions, providing families with access to the latest healthcare resources. CHF presently endorses services in several significant places, such as: Delhi/NCR Siliguri (West Bengal) Jalandhar (Punjab) Guwahati (Assam) The treatment for Pulmonary Hypertension typically involves a multi-faceted approach, which may include medications, oxygen therapy, and in some cases, surgical interventions. The cost of treatment can vary widely depending on the severity of the condition and the chosen treatment plan. In India, the approximate cost for managing Pulmonary Hypertension can range from ₹1 lakh to ₹5 lakhs annually, depending on the type of medication and treatment required. This financial burden can be overwhelming for many families, especially those from underprivileged backgrounds. It is important to identify and promptly treat Pulmonary Hypertension as a serious condition. Families are being supported by the Child Heart Foundation to navigate through this trying time. Our mission is to assist those suffering from heart disease by providing free medical care to disadvantaged children and financial assistance to others. We are here to help if you or someone you know has Pulmonary Hypertension. Call today!
World PH Day: Action Follows Awareness
World Pulmonary Hypertension Day, annually celebrated on the fifth of May, highlights the global impact of Pulmonary Hypertension (PH) - a lethal hemodynamic and pathophysiological disease, that affects a large number of children and adults worldwide. As a student intern at Child Heart Foundation, I’ve had the opportunity to explore the nuances of this chronic respiratory disease, by analysing medical research papers, case studies of patients, along with its poignant statistics (reduced life expectancy and appalling death rate).
Pulmonary Hypertension is described as the abnormal increase in pressure of the arteries present in the lungs. The most common kind of PH involves the pruning of the Pulmonary Artery, thus disrupting the physiological process of blood circulation. While the muscular walls of the Right Ventricle face immense pressure and weaken, the Left Auricle and Ventricle of the heart receive paucity of blood, resulting in a myriad of complications. Based on aetiology, the World Health Organisation has classified PH into five distinctive groups - which has further stimulated case-based research, as well as aided in customized patient care. However, the primary cause of such a life-threatening disease remains unknown, and is daunting from a psychosocial perspective.
In my perspective, one of the biggest challenges in PH management is the lack of awareness - given the fact that symptoms are generic, and are not specific to PH. This ultimately leads to delay in diagnosis. In most developing countries, the disease is either underdiagnosed or misdiagnosed. One should always be aware of alarming symptoms, such as cyanosis (bluish tint on lips and skin), dyspnea (shortness of breath) and syncope (fainting spells) and seek immediate medical help. Furthermore, one should also be aware of risk factors that could instigate the disease, such as smoking, the usage of illegal drugs and obesity.
The abovesaid, treatment is not freely accessible in developing countries, and is prohibitively expensive (approximately five lakhs), which along with lack of awareness, makes PH a fatal disease. Further, not all major drug companies are interested in these developing markets, which further accentuates the challenge of free accessibility of medication.
Action follows Awareness - Local fundraising, International Charity Programmes, and the involvement of authorities and governmental bodies seem plausible only when enough awareness has been created in communities. In order to achieve the aforementioned objective, it is indispensable to encourage the world in bringing more advocacy/research and setting up infrastructure for the treatment of PH. With the ongoing COVID 19 Pandemic, the significance of global health cannot be better exemplified.
This World PH Day, I urge you to take the first step - the onus of spreading awareness lies within you. Be a global citizen. Educate yourself, your family/friends, and caregivers, and seek timely medical aid on the onset of symptoms. This is the first stride towards a world of healthier and disease-free lungs.
Written by Richa Thyagarajan, Interning with Child Heart Foundation
Richa Thyagarajan is a Grade 11 Biology student from Bangalore, who aspires to become a Cardiothoracic Surgeon in the future. She enjoys making a difference in the lives of children, and has prior experience working in an NGO setting

Little Anaya Gets a new Life !
When the pandemic was at its peak and the country was under a lockdown. Anaya was born to parents Aasif and Praveen in Shahdara, New Delhi. She was born on the date 28/05/2020. Her birth time was quite a struggle for the parents as there was no bed available in the hospitals.
Finally, in Swami Dayanand Hospital a bed was available where Anaya’s mother got admitted 2 days before her birth. Anaya was doing fine till the first two months of her birth. After the second month she started showing symptoms of breathlessness. It was very hard for her parents to feed her anything.
The worried parents started taking Anaya to various private and government hospitals for treatment. Finally someone suggested taking her to Chacha Nehru Bal Chikitsalaya. She was admitted there for 15 days. They did multiple X-Rays and CT scans, where they suspected cardiac abnormality , as they had no Echo diagnostic facility , they referred her to CHF. Anaya needed to get a surgery done in a short time as her weight was falling drastically.
Her father had lost his job due to the pandemic and they were surviving on their savings and borrowing money from their relatives. They were extremely worried at the moment as they did not have sufficient funds for doing the treatment for Anaya.
Anaya first visited CHF on 2nd February 2020 to get a screening test done. She was diagnosed with Double Aortic Arch and the intervention for this included Double Aortic Arch Repair. Anaya was registered for surgery and her fundraising process began.
The time in between her screening and her treatment was extremely challenging for Anaya. She constantly had fever and stayed up throughout nights. It was difficult to feed her anything. They have also visited the emergency room at the nearest government hospital multiple times for seeking treatment. The team at CHF provided them continuous support over the telephone for monitoring Anaya’s health.
Through the support of a number of Donors on April 2nd 2021 Anaya was finally admitted for surgery at a hospital with required expertise for the diagnosed CHD and the best pediatric cardiology infrastructure. Her surgery occurred the next day from morning 9 am till 12:30 pm. She was discharged after a couple of days from the hospital.
Anaya is recovering quickly now and has also gained weight.
Her Father says “The birth of Anaya was a blessing for us. I wasn’t able to see the state my baby was in. I would heartily want to thank the donors for whom my baby was able to recover from this so quickly”
Story of Heart Warrior Anmol
2020 has been a hard year for all of us, some families along with fighting the virus also had to fight many personal battles in various forms, this is one such story. In the perilous times of the pandemic, Sunil Kumar’s family was under tremendous pressure as they had lost their only means of livelihood until a ray of hope came into their lives. Anmol was born on the 20th of May 2020. This was when the pandemic had started moving towards its peak. 4 months into his birth, he was unwell due to cold and fever. During that time, when Anmol’s mother was feeding him one day, she found him uncomfortable, sweating, and his heart beating really fast. She was extremely worried and took Anmol to the nearest dispensary where the doctor informed them that Anmol was very sick and was diagnosed with Pneumonia. The doctors also told them that Anmol had Down syndrome. Down syndrome is a genetic disorder that causes developmental and intellectual delays. The doctor asked the parents to take him to Pushpanjali hospital situated in Agra. The doctors prescribed lots of medicines that helped Anmol. Anmol’s father had to spend around 15,000 for one day for his treatment and all the tests done. A team of doctors had come to Pushpanjali to treat the COVID 19 patients. Suspecting some cardiac issue, they suggested Anmol’s father take him to Sri Sathya Sai Sanjeevani Hospital in Palwal, Haryana. They did an Echocardiography test in the hospital. As the case seemed complicated, he was referred to AIIMS. He was confirmed with heart disease but the treatment date was not given and due to pandemics, things were getting difficult.
Days went by and Anmol started getting sick by the hour, He used to constantly have colds, vomit, and was severely underweight. His parents' anxiety was increasing every day as they felt helpless. This was the time when Anmol’s father turned to the internet and started doing web searches about hospitals and organizations that could help him with his problem. This is when he stumbled upon the website of Child Heart Foundation. Given his experience from the past, he was extremely skeptical about traveling all the way to Delhi and returning with a negative response. He started watching youtube videos on CHF’s channel and was convinced about the services. He called our office and booked an appointment.
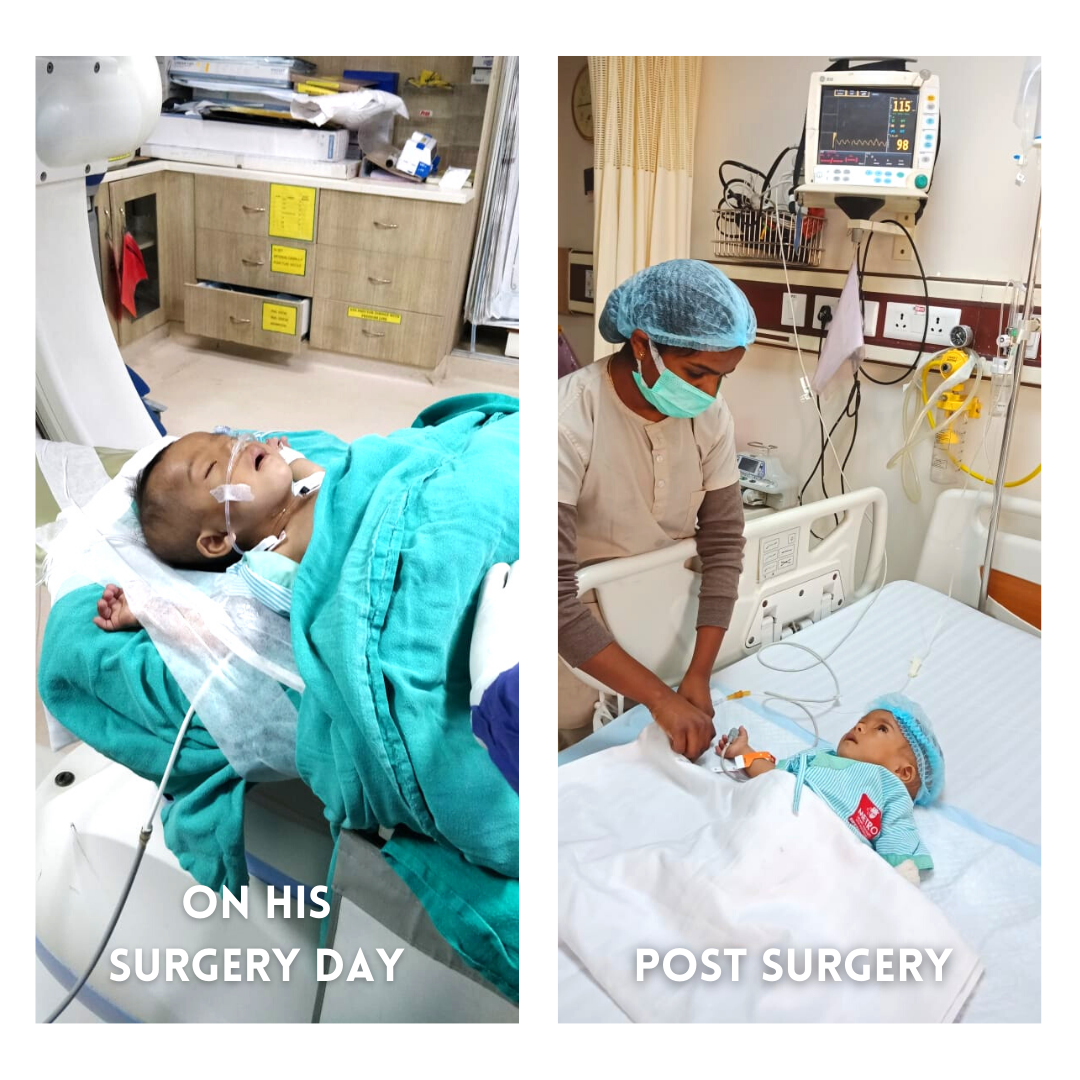
Anmol first visited CHF on the 19th of December, 2020. He got a free Echocardiography test done and was diagnosed with Patent Ductus Arteriosus (PDA). Dr. Vikas Kohli suggested that Anmol had to get a PDA device closure. The estimated surgery cost was around 1,90,000. His parents got really worried hearing about the treatment cost as Anmol’s father had lost his job during COVID and his past treatment had exhausted him financially. CHF assured them that the funds would be raised and they would be contacted when the concerned hospital gives them a date. They traveled back to Agra from Delhi.
The time in between Anmol’s first consultation to his intervention was a real battle for the family. Anmol had repeated occurrences of fever, vomiting and there were constant issues during feeding. His mother was in constant touch with CHF staff and gave repeated instructions on feeding like getting a steel Paldai and feeding milk through it. She was also given a diet chart to fulfill Anmol’s nutritional needs. As young parents, they were relatively less aware and were always high on anxiety as they used to call the team at every step for instructions. Our team was present for the family 24x7 overcall. They even didn’t know who the local pediatrician was and the place to get a COVID test done. Our team also helped them get attested the income certificate as Anmol’s father was scared by the fact that the MLA had to sign it. There were also times when their travel has gotten delayed due to many external factors. But the costs were partially covered by CHF.
Their long journey of 2 months, with every step of helplessness and anxiety experienced by the parents, with constant support by the team at CHF they learned to deal with the phase with maturity. The amount of 1,33,000 was raised by CHF with Delhi South Rotary Foundation and got Anmol treated at Metro hospital, Delhi.
His surgery was successful and after a couple of days, he was discharged from the hospital. He is doing very well now and has also started gaining weight.
Anmol’s father says- “I would like to extend my heartfelt thanks to the team at CHF and DSRF as they have been really supportive towards us in the past and have driven our fear away and helped Anmol get a new life and become a healthy child”
We at CHF, thank DSRF for helping us in treating Anmol.
Stay Connected
Stay connected for updates, insights, and exciting news delivered directly to you.